Cashless Facilities

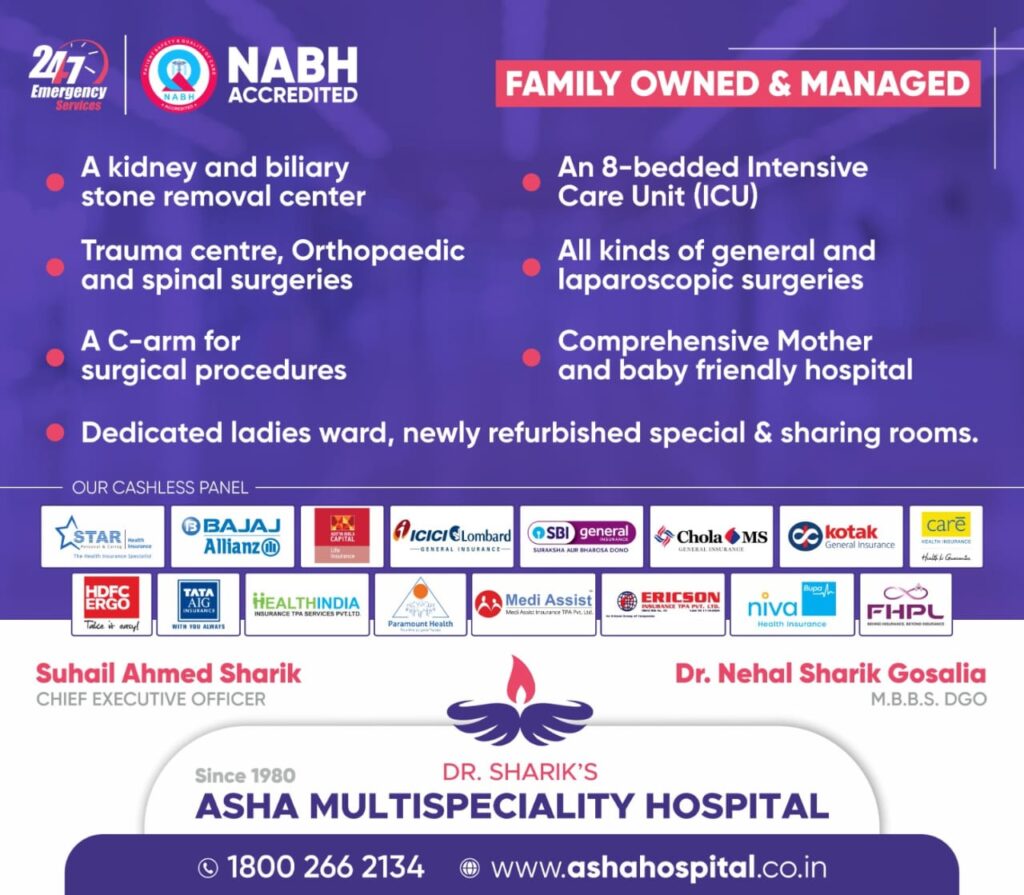
Our Partners














HOW TO OBTAIN CASHLESS FACILITY
Important: We request all members who want to avail cashless benefit to kindly call up our Helpline / Call Centre and confirm their policy service status & hospital network status.
- Insured has to arrange for the Request for Authorisation letter to be sent across from respective network hospital to THE TPA
- Request for Authorisation letter is available at admission counter / TPA Desk of network hospitals.
- The Request for Authorisation letter is to be filled in by the treating Doctor with his signature & stamped by the Hospital.
- It is mandatory for insured to mention the MDID Number on the request for proper identification / verification & further processing.
- It is mandatory for Insured to thoroughly check the request letter (to ensure that all required details are furnished & holds true to the best of their knowledge) & duly signing it as a confirmation.
- Above mentioned points are very important for registration of claim & further processing.
- Send the Request for Authorisation letter .On receipt of the completely filled request for Authorisation letter, the claim will be registered & a unique claim number called CCN will be generated. All correspondence will be against specific CCN for that particular hospitalization.
- In case there is a deficiency, it will be raised in the form of an additional document request & faxed to respective Hospital. The query & claim status can be obtained from the Hospital itself or Call Centre or on
- On receipt of deficient documents, the claim will be reviewed & processed further on as per admissibility.
- The denial of authorization for cashless access does not mean denial of treatment and does not in any way prevent you from seeking necessary medical attention or hospitalization.
- Cases wherein the claim is denied for cashless benefit Claimant / Insured can send all the claim documents for reconsideration in reimbursement along with the claim form.
IN CASE OF PLANNED HOSPITALISATION (to a Network Hospital)
- Kindly send the completely filled Request for Authorisation letter either by Fax or by E-Mail.
- Claims are processed at out head Office at Pune location and information pertaining to the claim status / information can be obtained from our local MDI office or the helpline.
- If the ailment is covered under policy conditions, an authorization Letter would be issued to the concerned hospital enabling you cashless facility.
- In case of any deficiency or query, an additional documents request will be sent to the Hospital. On receipt of the said information the request will be processed accordingly. If the ailment is not covered under policy terms and conditions, Denial will be sent to the hospital.
WHAT TO DO IN AN EMERGENCY?
- In an accidental case or in medical emergency you are advised to approach nearest Network / Non Network Hospital with your TPA DETAILS.If the admission is in a network hospital, pre-intimation can be made by the claimant or relatives by calling up our call center which is open 24 X 7.
- However it is still mandatory to send request for authorization letter for processing & consideration of case under cashless benefit.
- Private Limited will verify the coverage (both insurance & medical aspect) and if covered, issue the authorization letter to the network hospital.
Non Network Hospital
- If you are in a non-network hospital, you may pay the expenses and claim reimbursement based on policy coverage.
- You may get admitted as per the rules of the Hospital and make payments for the treatment taken and later on submit all the documents for reimbursement.
IN THE HOSPITAL
- The network hospital you have chosen will treat you without asking for a deposit & payment of hospital bills will be up to the authorized amount, the maximum liability being limit of indemnity subject to the coverage under the applicable policy terms and conditions.
- The claims will be settled as per the agreed tariff & package prices notwithstanding the amount sanctioned.
- Certain tertiary care hospitals will ask for some nominal deposit as per their protocol irrespective of approval of cashless guarantee to take care of non-covered expenses.
- If you are required to buy medicine or pay for investigations done outside the hospital, kindly obtain proper Cash Memo / Receipt for payment made by you. (The same can be claimed under reimbursement following discharge).
- Certain charges such as (Telephone / Fax, Food & Beverages for relatives, Barber, Ambulance etc.) are not covered under your insurance policy. If you have obtained such services from the hospital please pay for the same directly to the hospital.
- The policy which you have purchased may also contain certain additional clauses like co-pay, room restriction, etc. which will be applied while sanctioning cashless. All such expenses need to be paid by the Insured to the hospital prior to discharge & will not be reimbursed as per the terms and conditions of the applicable policy.
AT THE TIME OF DISCHARGE
- The hospital will discharge you without payment of the bills, except non-payable expenses, on the basis of authorization issued.
- If the bill amount exceeds the limit of indemnity, you will have to pay the excess amount to the hospital.
- Network hospital, wherein you have availed cashless benefit, will not give you the Original Bill, Discharge Card, Investigation Reports, etc. (as they have to send these to MDIndia Health Insurance TPA Private Limited. However you may ask for copies of the same for your records & subsequent follow-up.
- Prior to discharge, the insured should verify the Final Bill & duly sign the same.
Procedure for Reimbursement cases
Reimbursement claims can be submitted to YOUR TPA through courier, post or In Person at any of branch offices.
Claim form can be collected from the nearest branch offices does not amount to admission of any liability, under the policy on the part of the insurers.
Documents that you need to submit for a hospitalization reimbursement claim are:
Claim form can be collected from the nearest branch offices does not amount to admission of any liability, under the policy on the part of the insurers.
Documents that you need to submit for a hospitalization reimbursement claim are:
- Original Completely filled in Claim form.
- Covering letter stating your complete address, contact numbers and email address (if available), along with Schedule of Expenses.
- Copy of theTPA I CARD.
- Original Discharge Card &/OR Summary.
- Original hospital final bill.
- Original numbered receipts for payments made to the hospital.
- Complete breakup of the hospital bill.
- All bills for investigations done with the respective reports.
- All bills for medicines supported by relevant prescriptions.
- Based on the processing of the claim, a pre-repudiation or Claim payment statement is executed. In case of Claim payment statement, a NEFT is executed for the settled amount.
- On receipt of claim a, Medical team at TPA will determine whether the condition requires admission and the treatment is covered by your Employee Insurance Policy. They will also check all the other terms and conditions of your Insurance Policy. Non-medical expenses will not be payable.
Note: Only expenses relating to hospitalization will be reimbursed as per the policy taken. All non-medical expenses will not be reimbursed.
How does one get Reimbursement for pre and post hospitalization expenses under this scheme?
- The medical expenses incurred prior to Hospitalization are called Pre- hospitalization expenses and those incurred Subsequent to discharge as Post Hospitalization expenses.
- Mediclaim Policy allows reimbursement of medical expenses incurred prior to certain days of hospitalization & up to a certain number of days after discharge, provided the ailment/ disease for which hospitalisation is covered under the policy Terms & Conditions.
These days are subject to the limits as described in your respective policy. For claiming all Pre-Post Hospitalization expenses,you need to send all bills in original with supporting documents in the following manner:
- Consultation bills should be supported with consultation note / papers of the doctor.
- Investigation / Pathological / Radiological test bills should be supported along with Reports & advice for the same.
- Chemist bills should be supported with respective prescriptions for the same.
- Copy of Discharge Card of the Hospitalization.
These documents can be submitted to nearest branch Office.
